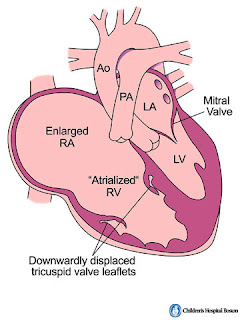
Ebstein's anomaly risk of anomaly 1 in 20,000 higher frequency in mothers who take lithium tricuspid valve leaflet anterior leaflet - largest leaflet and attached to valve annulus, large, redundant posterior and septal leaflet- vestigial/ absent - (failure of delamination of leaflets) when present the leaflets free edges are generally displaced posteriorly and downwards from AV junction and progressively towards the RVOT RV the RV i divided into two parts - proximal part - atrialized RV and distal part is RV proper and is small Different classifications to describe Ebstein's - type I--> IV (IV is the worst) Associated cardiac defects - ASD, PFO, VSD, PDA, RVOTO, Coarctation, WPW, LVNC Differential diagnosis of Ebstein's - tricuspid valve dysplasia - tricuspid valve prolapse - TV endocarditis - carcinoid heart disease - Uhl's anomaly - ARVC EKG findings RAE, RVH, RBBB, pre-excitation ECHO - TV displacement >0.8cm/m^2 of BSA com...